Abstract
Background Mortality rates and causes of death in children with sickle cell disease (SCD) have changed significantly over the past several decades. With ongoing improvements in standards of care, modern mortality rates and causes of death must be updated. Children's Healthcare of Atlanta (CHOA) houses one of the largest pediatric SCD programs in the country. This analysis reviews causes of death in children with SCD who were treated at CHOA between June 2010-June 2022.
Methods We reviewed the CHOA's Sickle Cell Clinical Database (SCCD) for deceased patients. Demographics, SCD genotype, date and age at death, healthcare utilization, hydroxyurea (HU) use, chronic transfusion therapy (CTT), and bone marrow transplant (BMT) were obtained from the SCCD. Cause of death and history of significant comorbidities were abstracted from the medical record, death certificates and/or autopsy reports.
Results A total of 4022 unique patients with SCD were seen at CHOA from June 2010- June 2022. Fifty-seven patients died during this period. All but 1 patient had been seen in the CHOA Sickle Cell Outpatient Clinic at least once. That patient received SCD care at a different institution, died from complications of a non-SCD related disease following transfer to CHOA, and was excluded from analysis.
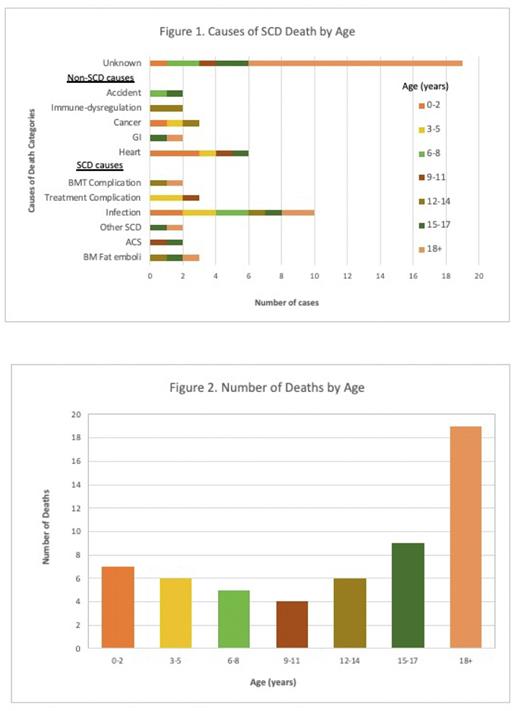
SCD-related causes accounted for 22 (39%) deaths. Acute SCD-related causes included bone marrow fat emboli, acute chest syndrome or pneumonia, cerebral hemorrhage in a person with history of stroke and moyamoya, and pulmonary hypertensive crisis. Of the infectious causes included Streptococcus pneumoniae, gram negative bacteria, unspecified streptococcal meningitis (by verbal report), and due to presumed septic shock complicated by severe anemia. Viral infections included respiratory syncytial virus, COVID-19 with severe anemia, and Parvovirus B-19 complicated by bone marrow fat emboli. Death due to complications of treatment included ceftriaxone-induced hemolysis and severe intrathoracic hemorrhage after apheresis catheter removal for treatment of ACS. BMT-associated complications included adenovirus infection after transplant with a matched unrelated donor and Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis after haploidentical transplant (see Figure 1).
Non-SCD comorbidities or accidents accounted for 15 (27%) deaths. These included heart disease, advanced cancer or complications of cancer (including E. coli sepsis in a child with relapsed neuroblastoma), accidents, one due to motor vehicle accident and one drowning. Gastrointestinal causes included bleeding from undiagnosed inflammatory bowel disease and liver failure leading to coagulopathy and intracranial hemorrhage. There was a case of severe anemia related to systemic lupus erythematosus.
The causes of death were unknown in the remaining 19 (34%) of individuals. Six (11%) were under 18 years of age. Five died at home or out of state and had no autopsy information, one had autopsy declined by the coroner. Of those who were 18 years of age or older, 7 (53%) were lost to follow-up, 3 (23%) had transitioned to adult care, and 3 (23%) were still being treated at CHOA.
There were more deaths in the 0-2 year and 15-17 year groups, and the most among adults (n = 19, 34%). Death from congenital heart disease was more frequent in children 0-5 years old. Pneumococcal sepsis were in children 5-7 years old, after stopping penicillin and before the second Pneumovax vaccine. Other bacterial infections were evenly distributed by age. Non-infectious SCD-related deaths were more likely to occur in patients 12 years and older (n = 6, 86%) (Figure 2).
Conclusions Continuing from a previous study by Lai et al. (2020) which reported the 10-year mortality rate at CHOA, this study described the causes of death of SCD patients during a 12-year period. Of direct SCD-related causes, bone marrow fat embolism was the most common and was also present in a patient who also had Parvovirus-B19 infection. Severe anemia was present in several patients at the time of death, associated with ceftriaxone-induced hemolysis, presumed septic shock, COVID-19, systemic lupus erythematosus, as well as G or intracranial hemorrhage. Patients beginning transition to adult care are at risk of becoming lost to follow-up and may experience difficulties transitioning to adult care. Future analyses will include review of regional hospital where available, and CDC's National Death Index.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal